The credit balance process in medical billing is a critical component of healthcare revenue cycle management. A credit balance occurs when a patient or insurance payer has paid more than the actual amount owed for medical services. If not identified and resolved promptly, credit balances can lead to compliance risks, delayed refunds, patient dissatisfaction, and potential audits. An efficient credit balance management process helps healthcare providers maintain financial accuracy and regulatory compliance.
What Is a Credit Balance in Medical Billing?
A credit balance appears on a patient’s account when payments exceed charges. This can occur due to:
Duplicate insurance payments
Overpayments from patients
Incorrect charge entry
Coordination of benefits (COB) errors
Claim processing or posting mistakes
Credit balances represent money that does not belong to the provider and must be refunded or corrected.
Importance of Credit Balance Management
Proper credit balance handling is essential for:
Ensuring compliance with CMS and payer regulations
Preventing government and payer audits
Improving patient trust and satisfaction
Maintaining clean and accurate accounts receivable
Avoiding financial penalties and legal issues
Healthcare organizations are required to identify and resolve credit balances within a specified timeframe, making this process highly important.
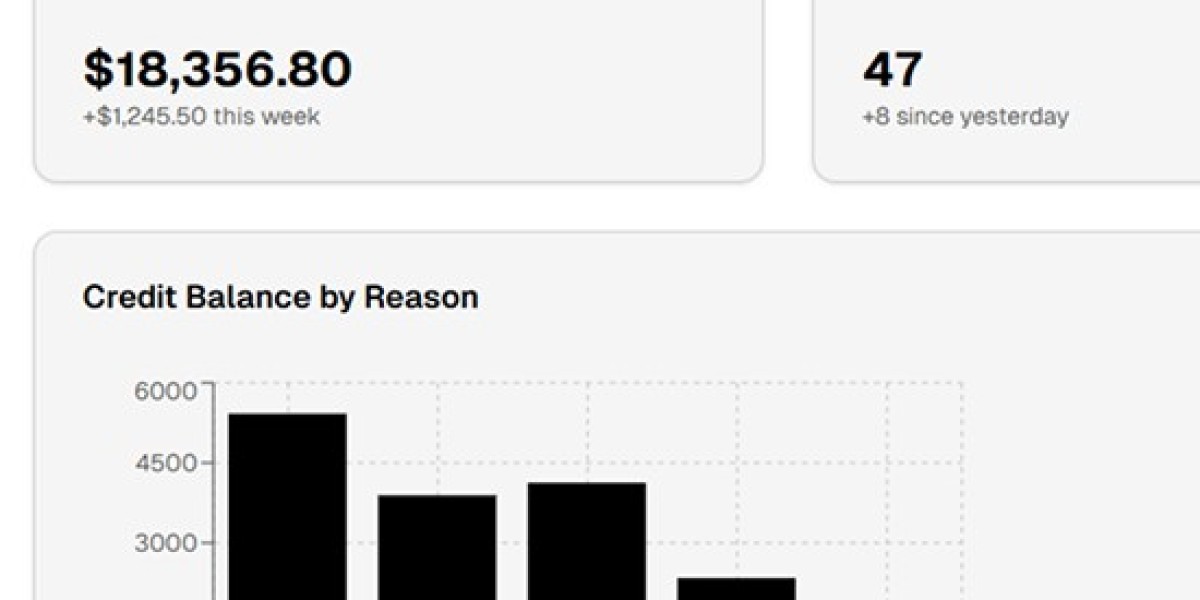
Step-by-Step Credit Balance Process in Medical Billing
1. Credit Balance Identification
The first step is identifying accounts with credit balances through regular system reports or billing software. These reports help billing teams flag overpaid accounts quickly.
2. Account Review and Analysis
Each credit balance account is reviewed to determine the root cause. This includes verifying:
Original charges
Payment sources
Contractual adjustments
Insurance explanations of benefits (EOBs)
Accurate analysis prevents unnecessary or incorrect refunds.
3. Payer or Patient Responsibility Determination
After analysis, billing specialists determine whether the refund is owed to:
Primary or secondary insurance
The patient
Another payer due to COB issues
This step ensures refunds are issued to the correct party.
4. Correction and Adjustment
If the credit balance is due to billing or posting errors, corrections are made in the system. This may include charge corrections, payment reallocations, or claim resubmissions.
5. Refund Processing
Once verified, refunds are processed according to payer guidelines and internal policies. Proper documentation is maintained to ensure audit readiness.
6. Reporting and Compliance Tracking
Detailed records of resolved credit balances are maintained for compliance and reporting purposes. Regular monitoring helps prevent future credit balance issues.
Common Challenges in Credit Balance Processing
High claim volumes and limited staff
Complex payer refund rules
Inaccurate payment posting
Delayed identification of overpayments
Outsourcing credit balance services can help overcome these challenges efficiently.
Benefits of Outsourcing Credit Balance Services
Healthcare providers benefit from outsourcing by:
Reducing compliance risk
Speeding up refund resolution
Improving operational efficiency
Allowing internal teams to focus on core billing tasks
Experienced RCM professionals ensure accurate and timely credit balance resolution.
Conclusion
The credit balance process in medical billing plays a vital role in maintaining financial integrity and compliance in healthcare organizations. By implementing a structured credit balance workflow or partnering with a trusted medical billing service provider, healthcare practices can effectively manage overpayments, reduce risks, and improve overall revenue cycle performance.